Diagnostic and prognostic research
Emergency medicine involves the early recognition of critical illness and injury, and the risk stratification of patients to ensure that the most unwell are treated promptly. We know that the longer we delay the diagnosis and treatment of patients with rapidly evolving pathology, the poorer their eventual outcomes. Innovation in diagnosis and prognosis modelling is essential to prevent deterioration and promptly treat disease
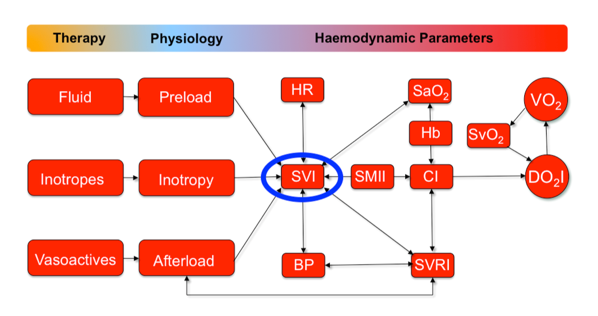
In the Emergency Department, patients present with diverse and undifferentiated medical conditions, and patients are diagnosed and treated depending upon their presenting problem. Risk stratification and rapid identification of critically ill patients is vital, as the immediate management and urgent treatment of patients presenting to the ED relies on prompt recognition. Currently, assessment of the patient’s haemodynamic status in the ED mainly depends on the measurements of physiological vital signs, however these vital signs may lack both sensitivity and specificity, as many variables change late in the course of evolving time-critical pathology, as our bodies strive to compensate for the disease and maintain cerebral oxygenation. When critically ill or injured patients are cared for in the intensive care setting, invasive monitoring methods allow direct measurement of central cardiovascular function, but emergency department patients have a similar urgent need to detect impending cardiopulmonary deterioration and shock during the early compensatory stage of haemorrhage, sepsis and other pathologies, in order to resuscitate patients and prevent poorer outcomes.
More direct monitoring of haemodynamic function, and therefore oxygen delivery, in patients presenting to the emergency department permits frequent measurement of core variables. There has been development and research into innovative non-invasive haemodynamic monitoring technologies, and these may offer new insights into rapid recognition of early compensation prior to haemodynamic collapse. A lack of studies in the emergency department setting investigating the measurement of pre-treatment haemodynamic parameters of time-critical patients mean that evaluation and assimilation of physiological data into the clinical decision-making process is cumbersome at best.
Previous work has only focused on selected, easily available variables in the assessment of fluid responsiveness, and minimal effort has been directed toward formal, rigorous examination of the relative importance of combining directly measured core parameters in the ED setting. The additive prognostic and predictive significance of the combination of multiple central haemodynamic variables, which can be collected by using innovative non-invasive monitoring remains to be studied.
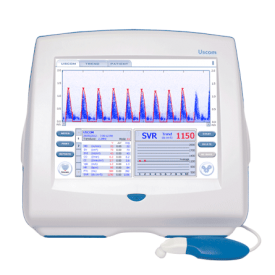
The aim of these projects is to evaluate the prognostic and predictive significance of a comprehensive selection of clinical and haemodynamic parameters derived from the Ultrasound Cardiac Output Monitor (USCOM) in a large, unselected, prospective cohort of emergency department patients of different ages and a wide range of pathologies.
“USCOM 1A is a non-invasive, transcutaneous Doppler ultrasound device designed to simplify acquisition and storage of high-fidelity measurement and trending information of cardiovascular performance. It uses state-of-the art electronics, high fidelity ultrasonics and advanced signal processing to deliver accurate and simple measurements of Cardiac Output”