CEDRIC
Comprehensive Emergency Dataset for Research, innovation and Collaboration
Recent Australian national data report just over eight million separate episodes of care over the preceding 12 months, increasing by 2.5% per year. After their resuscitation, diagnosis and treatment in the ED, including blood test, x-rays, CT scans and other investigations, around 40% or more of patients are admitted to hospital, with the rest discharged into the community; if admitted, it may be to a medical or surgical ward, intensive care, coronary care, or straight to the operating theatre or cath lab if their condition is life-threatening. Finally, after hospital stays, rehabilitation and multidisciplinary evaluation they may return home to the care of their family and their primary care team. This patient care journey however is contained within multiple databases and may only be analysed using complex database queries, involving multiple teams with multiple skill sets.
EDRIC evolved from the MEME database, which was designed to capture and link the data collected in the Electronic Medical Record (EMR) which has traditionally been in separate silos of information, meaning that the patient’s journey from Emergency Medicine through the hospital to discharge cannot be understood. As you can see on the MEME page, this is a retrospective database, soon to contain records of almost three million patient presentations across SWSLHD.
Linked data across the entire patient journey…
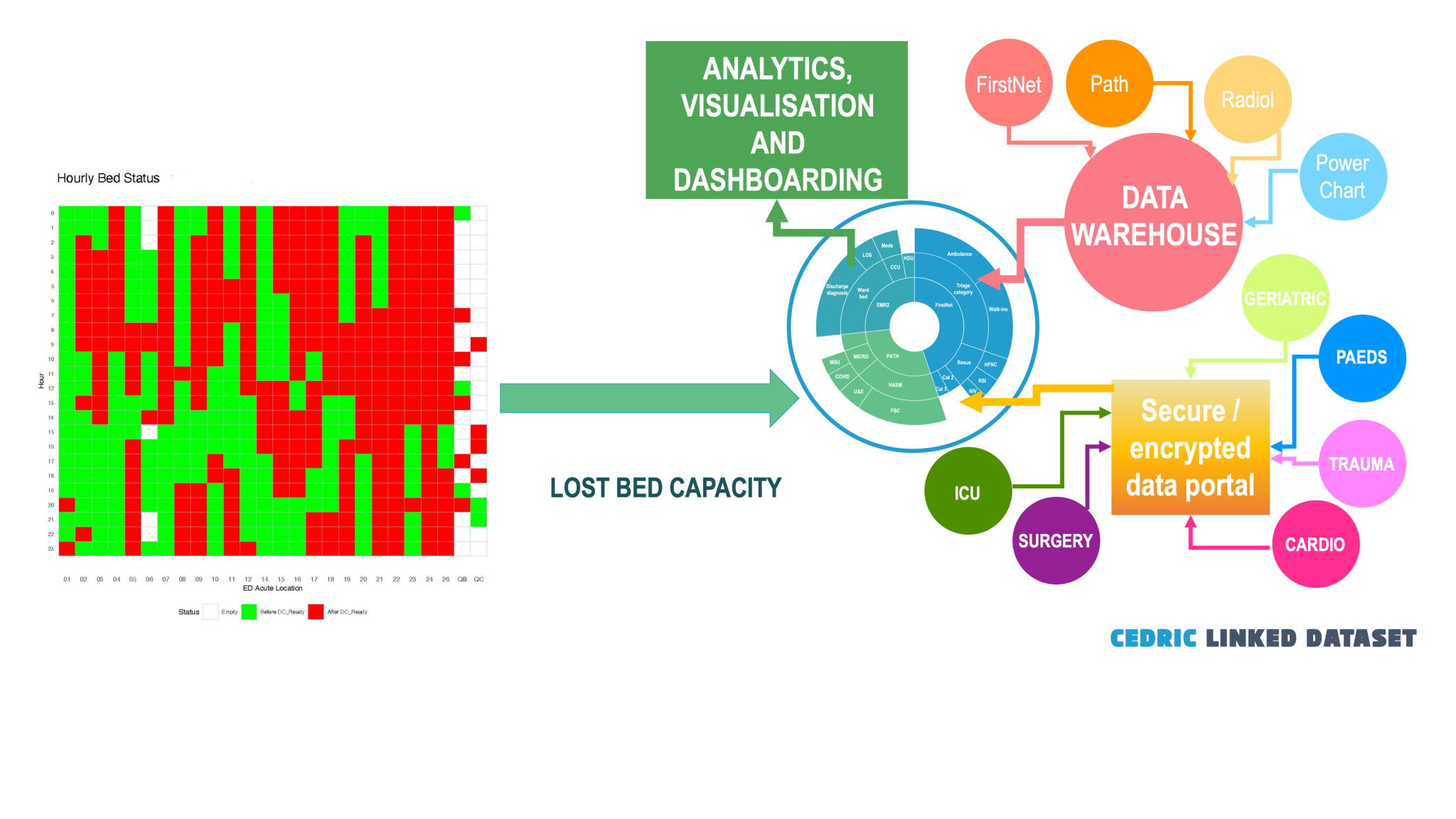
CEDRIC is a revolution in health data collection and use, as it draws data from the Cerner EMR, from the ED, wards, pathology and radiology, then links all datapoints together to give a prospective, continually growing database of detailed patient journeys. This allows researchers to follow the patient as they move through the healthcare system from the Emergency Department all the way to their discharge from the hospital

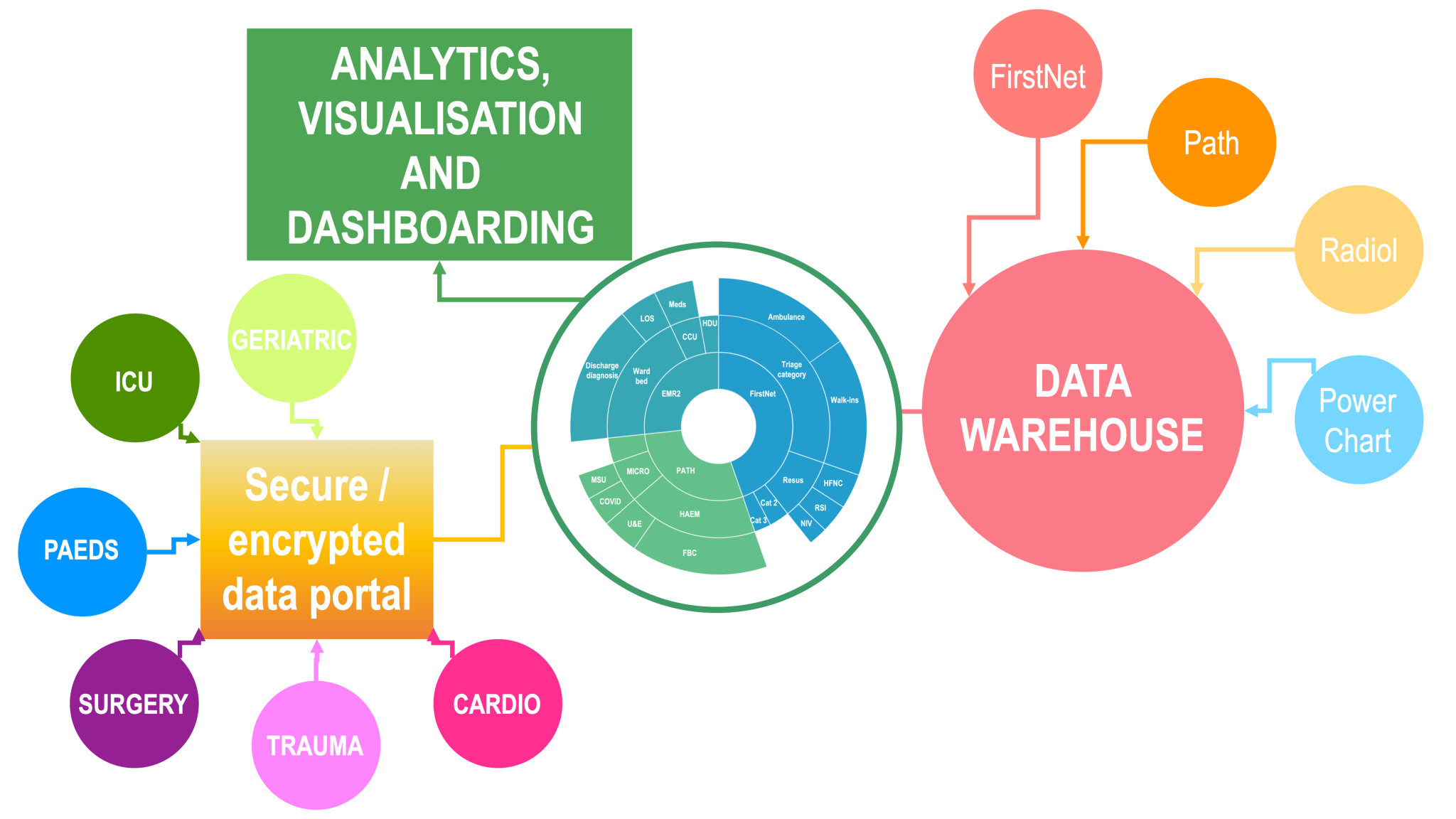
Bespoke databases for all specialties, linked to CEDRIC
That is only part of CEDRIC however; we plan to build a series of bespoke databases for clinical colleagues and their departments, not only making linked data available for their use in contemporary and evidence-based patient care, but will also make the data available to link to the rest of CEDRIC. The outcomes of this are that CEDRIC will contain not only the patient care information routinely collected into the EMR, but will also contain all the specialist investigations and procedures, including physiological data and images.
Machine learning, artificial intelligence and agent-based modelling
We plan to embed automated data analytics into CEDRIC, using cutting-edge techniques such as machine learning and other artificial intelligence approaches, to identify predictive models of disease outcomes, accurately identify patients most at risk of death or deterioration, and enable unparalleled insights into patient care

Unstructured data and patient monitoring
CEDRIC will take unstructured data such as the output from patient monitors, 12-lead ECGs, echocardiograms, CT and MRI, link the data to the patient records, and use supervised, unsupervised and deep learning to recognise patterns not discernible by humans. These analyses will be used to identify patterns in patient physiology representing normality, deterioration and critical illness and injury.
